KNOW YOUR OPTIONS
Deciding on the right vascular access device option for you goes far beyond the treatment itself—it may provide advantages to your lifestyle and comfort, as well as the long-term health of the veins in your hands and arms.
THE PORTREADY™ PROGRAM
The PortReady™ Program is a patient information initiative focused on helping you, or a loved one, as you start infusion therapy treatment. Infusion therapy isn’t always easy, but we believe choosing the right vascular access device is an important first step. The PortReady™ Program is a resource that provides you with information regarding port placement, port access, and care. The right information can help you to be PortReady™.
THE INFUSION THERAPY PROCESS
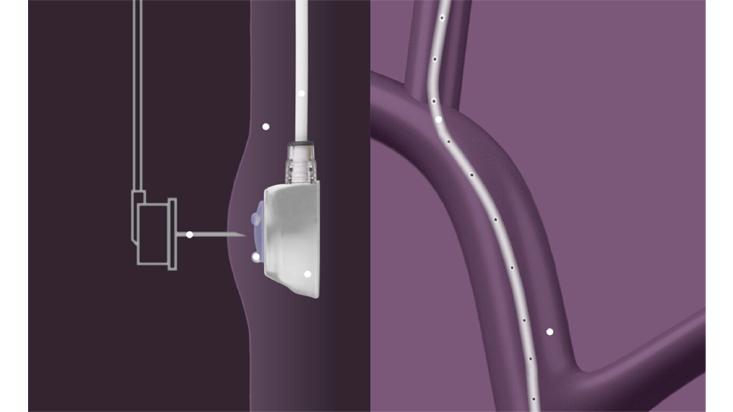
Intravenous (IV) infusion therapy is the delivery of medication or fluids through a catheter tube and into the vein. These tubes can be placed in veins of the hand or lower arm (peripheral I.V), or through devices such as a peripherally inserted central catheters (PICC), central venous catheters (CVC), or implantable ports. Talk to your healthcare provider about what’s best for you.